Higher dementia risk linked to more use of common drugs

Further evidence found of association between anticholinergics and Alzheimer's disease in University of Washington / Group Health study in JAMA Internal Medicine
SEATTLE—A large study links a significantly increased risk for developing dementia, including Alzheimer’s disease, to taking commonly used medications with anticholinergic effects at higher doses or for a longer time. Many older people take these medications, which include nonprescription diphenhydramine (Benadryl). JAMA Internal Medicine published the report, called “Cumulative Use of Strong Anticholinergics and Incident Dementia.”
The study used more rigorous methods, longer follow-up (more than seven years), and better assessment of medication use via pharmacy records (including substantial nonprescription use) to confirm this previously reported link. It is the first study to show a dose response: linking more risk for developing dementia to higher use of anticholinergic medications. And it is also the first to suggest that dementia risk linked to anticholinergic medications may persist—and may not be reversible even years after people stop taking these drugs.
“Older adults should be aware that many medications—including some available without a prescription, such as over-the-counter sleep aids—have strong anticholinergic effects,” said Shelly Gray, PharmD, MS, the first author of the report, which tracks nearly 3,500 Group Health seniors participating in the long-running Adult Changes in Thought (ACT), a joint Group Health–University of Washington (UW) study funded by the National Institute on Aging. “And they should tell their health care providers about all their over-the-counter use,” she added.
“But of course, no one should stop taking any therapy without consulting their health care provider,” said Dr. Gray, who is a professor, the vice chair of curriculum and instruction, and director of the geriatric pharmacy program at the UW School of Pharmacy. “Health care providers should regularly review their older patients’ drug regimens—including over-the-counter medications—to look for chances to use fewer anticholinergic medications at lower doses.”
For instance, the most commonly used medications in the study were tricyclic antidepressants like doxepin (Sinequan), first-generation antihistamines like chlorpheniramine (Chlor-Trimeton), and antimuscarinics for bladder control like oxybutynin (Ditropan). The study estimated that people taking at least 10 mg/day of doxepin, 4 mg/day of chlorpheniramine, or 5 mg/day of oxybutynin for more than three years would be at greater risk for developing dementia. Dr. Gray said substitutes are available for the first two: a selective serotonin re-uptake inhibitor (SSRI) like citalopram (Celexa) or fluoxitene (Prozac) for depression and a second-generation antihistamine like loratadine (Claritin) for allergies. It’s harder to find alternative medications for urinary incontinence, but some behavioral changes can reduce this problem.
“If providers need to prescribe a medication with anticholinergic effects because it is the best therapy for their patient,” Dr. Gray said, “they should use the lowest effective dose, monitor the therapy regularly to ensure it’s working, and stop the therapy if it’s ineffective.” Anticholinergic effects happen because some medications block the neurotransmitter called acetylcholine in the brain and body, she explained. That can cause many side effects, including drowsiness, constipation, retaining urine, and dry mouth and eyes.
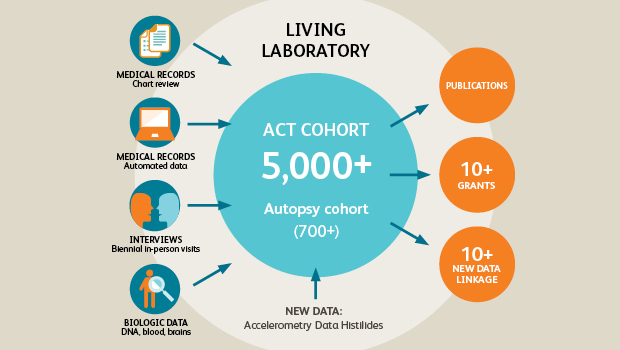
“With detailed information on thousands of patients for many years, the ACT study is a living laboratory for exploring risk factors for conditions like dementia,” said Dr. Gray’s coauthor Eric B. Larson, MD, MPH. “This latest study is a prime example of that work and has important implications for people taking medications—and for those prescribing medications for older patients.” Dr. Larson is the ACT principal investigator, vice president for research at Group Health, and executive director of Group Health Research Institute (GHRI). He is also a clinical professor of medicine at the UW School of Medicine and of health services at the UW School of Public Health.
Some ACT participants agree to have their brains autopsied after they die. That will make it possible to follow up this research by examining whether participants who took anticholinergic medications have more Alzheimer’s-related pathology in their brains compared to nonusers.
Drs. Gray and Larson’s coauthors are Paul Crane, MD, MPH, an associate professor of medicine at the UW School of Medicine, adjunct associate professor of health services at the UW School of Public Health, and affiliate investigator at GHRI; Sascha Dublin, MD, PhD, a Group Health physician, GHRI associate investigator, and affiliate associate professor of epidemiology at the UW School of Public Health; Melissa L. Anderson, MS, and Onchee Yu, MS, senior biostatisticians, and Rod Walker, MS, biostatistician, at GHRI; Joseph T. Hanlon, PharmD, MS, a professor of medicine at the University of Pittsburgh; and Rebecca Hubbard, PhD, an associate Professor of Biostatistics at the Hospital of the University of Pennsylvania, who did this work while on staff at GHRI.
This work was supported by National Institute on Aging NIH Grants U01AG00678 (Dr. Larson), R01AG 027017, R01AG037451, P30AG024827, T32 AG021885, K07AG033174 (Dr. Hanlon), and R03AG042930 (Dr. Dublin) and by the Branta Foundation (Dr. Dublin).
University of Washington School of Pharmacy
The UW School of Pharmacy is committed to educating the next generation of leaders in pharmacy, pharmaceutical research, and health care—while seeking to ensure the safe, rational, and cost-effective use of medicines. Founded in 1894, the UW School of Pharmacy is ranked #3 in the world according to Shanghai Jiao Tong University. Follow the School of Pharmacy on Facebook or Twitter.
UW Medicine
UW Medicine is part of the University of Washington. Its mission is to improve the health of the public by advancing medical knowledge, providing patient care, and training the next generation of physicians and other health professionals. Its system includes Harborview Medical Center, Northwest Hospital & Medical Center, Valley Medical Center, UW Medical Center, UW Neighborhood Clinics, UW Physicians, UW School of Medicine and Airlift Northwest. UW Medicine is affiliated with Seattle Children’s, Fred Hutchinson Cancer Research Center, the Veteran’s Affairs Healthcare System in Seattle, and the Boise VA Medical Center. It shares in the ownership and governance of the Seattle Cancer Care Alliance and Children’s University Medical Group.
About Kaiser Permanente
Kaiser Permanente is committed to helping shape the future of health care. We are recognized as one of America’s leading health care providers and not-for-profit health plans. Founded in 1945, Kaiser Permanente has a mission to provide high-quality, affordable health care services and to improve the health of our members and the communities we serve. We currently serve more than 12.4 million members in eight states and the District of Columbia. Care for members and patients is focused on their total health and guided by their personal Permanente Medical Group physicians, specialists and team of caregivers. Our expert and caring medical teams are empowered and supported by industry-leading technology advances and tools for health promotion, disease prevention, state-of-the-art care delivery and world-class chronic disease management. Kaiser Permanente is dedicated to care innovations, clinical research, health education and the support of community health. For more information, go to: kp.org/share.
Co-Researchers
Melissa L. Anderson, MS
Principal Collaborative Biostatistician
Onchee Yu, MS
Principal Collaborative Biostatistician
Rod L. Walker, MS
Principal Collaborative Biostatistician
Year In Review

10 ways we made a healthier world in 2018
Kaiser Permanente Washington research tackled problems like obesity, suicide—and care that doesn’t promote health.
Read about it in News and Events.
ACT study
ACT study: Long-running study of aging examines changes in Group Health patients over time
Drs. Larson and Crane co-lead Group Health-University of Washington collaboration learning how to promote healthy aging.
Media contact
For more on Kaiser Permanente Washington Health Research Institute news, please contact:
Bianca DiJulio
bianca.s.dijulio@kp.org
206-660-8333
After-hours media line: 206-448-4056



