Accountable Communities of Health have made strides
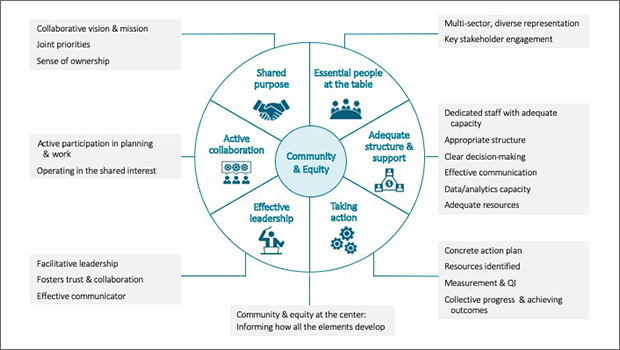
CCHE’s model for multi-sector collaboration is centered on community and equity.
With a new multi-sector collaboration model, Erin Hertel led CCHE’s evaluation showing ACHs can help make a Healthier Washington.
Awareness is growing that various social factors—like transportation, education, and race—can affect people’s health more than their health care does. Improving those factors for community health requires collaboration among people and organizations that may never have interacted before. But how can such disparate sectors work together effectively?
Drawing on years of experience evaluating community coalitions, Kaiser Permanente Washington Health Research Institute (KPWHRI)’s Center for Community Health and Evaluation (CCHE) created a model for successful collaboration to help answer that question. The model puts equity and the voice of the community at the center; other essential elements include shared purpose, active collaboration, effective leadership, essential people at the table, adequate structure and support—and taking action.
The team, led by Erin Hertel, MPA, describes this model in the report of their four-year evaluation of the development and impact of nine regional, multi-sector collaborative organizations called Accountable Communities of Health (ACHs). At the heart of the Washington State Health Care Authority’s Healthier Washington initiative, these ACHs aim to enhance the health of state residents, improve the quality of care, and reduce health care costs.
Largely successful to date
“Each of the ACHs chose which health challenge to tackle, but we found that they all have been largely successful to date in building strong collaborative organizations,” says Ms. Hertel, a senior evaluation and learning consultant at CCHE. “All of them have been awarded funding by Washington state, and they are poised to innovate in strategic ways—and improve the health of people throughout our state.”
Their approaches vary, but Washington ACHs have all:
- Built trust and collaboration,
- Established the infrastructure and capacity to implement large-scale system change,
- Created a comprehensive, integrated approach to health system transformation, and
- Incorporated community voice, equity, and the social determinants of health.
With $7.3 million in State Innovation Models, or SIM, federal funding, the ACHs were modestly resourced when they launched. But then Washington state started participating in a five-year, $1.1 billion Medicaid Transformation demonstration with the Centers for Medicare and Medicaid Services. The ACHs had evolved into independent organizations, which the state chose as its partners to support the state’s goals of better health, better care, and lower costs.
ACHs involve a disruptive new way of working, Ms. Hertel stressed: simultaneously top-down and bottom-up, driven by the state and each region and local community. “System transformation is disruptive, not more of the same—with the exception of continuing to be rooted in evidence-based practices such as the Chronic Care Model and the Patient-Centered Medical Home,” she says.
Most disruptive have been changes in how the system coordinates care across both clinical settings and social services. Many ACHs are putting some of the Medicaid Transformation funding into social wellness pools and moving it upstream, for instance, to help address other needs in the community such as food, housing and transportation.
“Several ACHs are doing set-asides or acting as grant makers themselves as needs arise for their communities,” says Michelle Chapdelaine, MPH, a CCHE evaluation and learning associate.
Going forward
Washington’s experience provides useful lessons for other states investing in large-scale collaborations to improve health:
- New state agency approaches and capacities are required to work effectively with regional partners.
- State agencies should seek a balance between state guidance and community solutions.
- A funded development period proved critical for building the foundation needed when greater health system transformation resources became available.
Now CCHE is continuing to work individually with two of the ACHs on how to design evaluations to understand their interventions. Meanwhile, CCHE is using the collaboration model in other projects, such as the national Strong, Prosperous, And Resilient Communities Challenges initiative, or SPARCC.
“The ACHs continue to evolve,” says Allen Cheadle, PhD, a senior investigator at KPWHRI. “In future, much of what the ACHs have been doing will have ripple effects beyond Medicaid.”
In addition to Ms. Hertel, Ms. Chapdelaine, and Dr. Cheadle, the ACH evaluation team also includes CCHE Senior Evaluation and Learning Consultant Lisa Schafer, MPH, and CCHE Evaluation and Learning Associate Carly Levitz, MPH. A State Innovation Model grant from the Center for Medicare and Medicaid Innovation funded CCHE’s assessment of the ACHs’ development, operations, and effectiveness.
By Rebecca Hughes
The CCHE team

We're known for our customized evaluations
Our team’s background spans a number of fields, including public health, economics, urban planning, epidemiology, and health administration.

CCHE uses strategic learning to evaluate Accountable Communities of Health
Rapid-cycle feedback is key as Erin Hertel leads Center for Community Health and Evaluation assessment of innovative Washington ACHs

SPARCC learns from communities about improving racial equity
Mid-project report on a 6-region initiative shows steps forward in prioritizing equity in community development

Center for Community Health and Evaluation
Our mission is to improve the health of communities with collaborative approaches to planning, assessment, and evaluation


