For mammography, radiologists do better without computer help
Based on a new BCSC study, Dr. Diana Buist tells of technology that adds cost to breast cancer screening—without improving outcomes. Dr. Marc Mora comments.
By Diana S.M. Buist, PhD, senior investigator at Group Health Research Institute (GHRI).
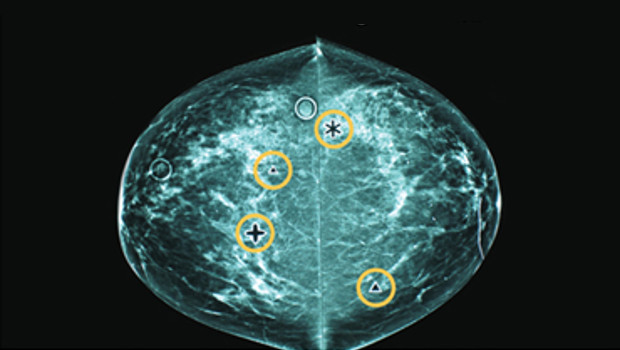
Usually, technology makes our world safer, our lives easier, and our health better. But not always. An example is computer-aided detection (CAD) to help radiologists find breast cancers. It sounds like a great idea. CAD software points out worrisome breast lesions on screening mammograms that a radiologist should look at more closely. If CAD helped detect cancers that a radiologist would likely miss, it would be worth the $400 million it adds annually to the national cost of mammography.
However, my colleagues at the Breast Cancer Surveillance Consortium (BCSC) and I have a new study that shows that CAD does not help radiologists find breast cancers. JAMA Internal Medicine published “Diagnostic Accuracy of Digital Screening Mammography with and without Computer-aided Detection,” and you can also read our news release.
The study, led by Constance Lehman, MD, PhD, found that not only does CAD add to the cost of mammograms without helping find cancers; it may result in more missed cancers. Dr. Lehman recently became the director of breast imaging at Massachusetts General Hospital in Boston and is an affiliate researcher at GHRI. Other coauthors include Diana Miglioretti, PhD, and Robert Wellman, MS.
"This is an important finding that all health systems will be looking at closely," Dr. Marc Mora, chief medical officer at Group Health, told me.
Our CAD study
CAD is not a brand-new technology. The Food and Drug Administration approved its use in 1998. The Centers for Medicare and Medicaid Services increased CAD reimbursements in 2002 even though then—as now—no evidence showed that CAD improves mammography accuracy. We found that CAD is now nearly standard: By 2012, more than 80 percent of mammograms in the BCSC dataset we used for our study were interpreted with CAD.
Other studies hinted that CAD doesn't improve a radiologist's ability to find breast cancers. We built on these earlier smaller studies with a large study on breast cancer screening as it is most often performed today: as digital mammography on a diverse population of women by radiologists familiar with CAD.
Using BCSC data on breast cancer screening done all over the country, we looked at the accuracy of digital screening mammography, measured by how often cancers were detected, how often they were missed, and how often an abnormality that was not a cancer was incorrectly labeled as one. We had data on mammograms read by 271 radiologists at 66 facilities across the United States—nearly a half-million mammograms with CAD and nearly 130,000 without. The mammograms were from more than 300,000 women who had the procedure between 2003 and 2009. We considered factors like differences in women's ages and radiologists' experience with CAD.
Our bottom line: The accuracy of screening mammography was not improved with CAD. Whether radiologists used CAD or not, cancer was detected in about 4 of every 1,000 women. With or without the software, about 3 in every 1,000 women were found to have invasive cancer.
The BCSC had enough data for us to compare screening accuracy when the same radiologist did or did not use CAD. This addressed concerns about different overall performance between radiologists who use and don’t use CAD. Our results suggest that CAD actually reduced the ability to detect true cancers. From other studies, we know this might be because CAD does not detect every cancer, and radiologists might pay less attention to an abnormality that CAD overlooked.
National health policy leaders will hear about this work
We concluded that CAD simply does not help detect breast cancer, even though CAD is used to interpret most mammograms. Our research team will be working to ensure that Medicare leaders and others who make policy and coverage decisions are aware of this important study.
Here at Group Health, we will continue to lead in breast cancer screening research through our involvement in the BCSC. As part of the BCSC, we have worked for two decades to figure out how to deliver the best breast cancer screening—and by best, I mean screening with the greatest benefits and the least harms to women.
"BCSC studies have a major impact on national guidelines and the evidence-based care we strive for at Group Health,” Dr. Mora told me. “We're glad to be a part of the BCSC." He says our work is a great of example of how breast cancer screening research at GHRI in conjunction with the BCSC helps Group Health make the best possible decisions about where to point our resources—ensuring we use member dollars wisely to deliver real and important improvements in screening.
I'm proud to be part of important work nationwide and here at Group Health to improve the value of our care. The way we use our health care resources affects our copayments and other out-of-pocket costs as Group Health members. That's why we're watching out for procedures that do not lead to better prevention, diagnosis, or treatment. Our CAD study is just one example of how Group Health contributes to national work to increase high-value health care for everyone.
Read more about improving the value of health care through the Choosing Wisely campaign.
Related News

What’s next for Choosing Wisely?
Dr. Buist helps set course for giving people needed care.



