A research team led by Dr. Michael Parchman uses new ways to support small clinics in reducing opioid use in the rural Pacific Northwest.
Researchers at Kaiser Permanente and the University of Washington (UW) have developed an innovative program to provide small rural clinics with practice support to reduce patients’ use of opioids.
The Annals of Family Medicine published their report, “Team-Based Redesign of Opioid Medication Management in Primary Care: Effect on Opioid Prescribing.” The research, funded mainly by the Agency for Healthcare Research and Quality (AHRQ), is part of Kaiser Permanente’s commitment to improve the health of the communities it serves.
Lead author Michael Parchman, MD, MPH, a senior investigator at the MacColl Center for Health Care Innovation at Kaiser Permanente Washington Health Research Institute, describes the Six Building Blocks, their results, and what’s next:
Q: Why focus on small, rural, primary care practices?
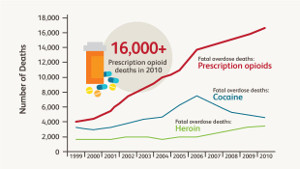
Michael Parchman: Opioids tend to be prescribed more often and in larger amounts in rural areas compared to cities and suburbs—and the epidemic’s most devastating effects have been in rural, disadvantaged populations. Most opioid prescriptions for chronic pain are provided in primary care. Larger integrated delivery systems like Kaiser Permanente have worked to lower opioid prescribing. But smaller clinics serving disadvantaged rural populations often have fewer resources—and their workforce is limited, as I learned when I practiced family medicine in rural Texas. That’s why we developed the Six Building Blocks.
Q: What are the Six Building Blocks?
MP: They comprise six common elements for team-based redesign of opioid medication management in smaller primary care settings:
- Provide supportive leadership and build consensus;
- Revise, align, and implement clinic policies, patient agreements, and workflows;
- Track and monitor patient care;
- Prepare for planned, patient-centered visits;
- Develop resources for “complex” patients with more needs; and
- Measure and celebrate success.
All our materials are online, publicly available, and free, and our website provides implementation guidance. The Six Building Blocks program has been adopted and/or recommended by the Washington State Department of Health and used by the Centers for Disease Control and Prevention (CDC) and Washington state's Bree Collaborative. The Oregon Health Authority has adapted them for their work on overprescribing. The Six Building Blocks were designed to improve opioid prescribing to align with evidence-based clinical guidelines.
Q: Why aren’t guidelines enough?
MP: It’s great that current guidelines support more judicious use of opioids for chronic pain, aiming to improve care’s safety and effectiveness. But educating individual providers about guidelines isn’t enough. To have a fighting chance of solving the opioid crisis, we must restructure how health care teams work together. We need a systematic, team-based approach to redesigning care, supported by changes to clinic systems and team workflows across entire clinics, as in the Six Building Blocks.
Q: What did you learn?
MP: We saw modest but significant improvements: The number of patients prescribed daily opioids long-term for chronic pain declined by 14%. The proportion on higher daily doses of opioids (100 morphine equivalent dose or higher) fell, from 11.8% to 9.6%. And participating providers and staff told us this program significantly lowered their work stress and made their work lives easier.
We worked for 15 months with six rural-serving organizations, including 20 clinics, in eastern Washington and central Idaho. They are part of the UW’s Washington, Wyoming, Alaska, Montana, and Idaho (WWAMI) region Practice and Research Network (WPRN). Comparing their patients to a control group in the same areas, we concluded that implementing the Six Building Blocks accelerated an existing trend to prescribe lower doses of opioids.
Q: What’s next?
MP: Since we’ve seen success in rural settings, we’ve started testing the Six Building Blocks in a more diverse group of primary care clinics, and the program may be relevant for them as well.
I must thank my coauthors: Robert B. Penfold, PhD, and Michael Von Korff, PhD, of KPWHRI; Laura-Mae Baldwin, MD, MPH, David Tauben, MD, Kari A. Stephens, PhD, and Brooke Ike, MPH, of the UW; and Mark Stephens of Change Management Consulting, in Seattle. The National Center for Advancing Translational Sciences of the National Institutes of Health (UL1 TR002319) provided additional support for our work.