What works to meet complex needs in diabetes care?

An ACT Center partnership is helping a nonprofit engage patients and provide comprehensive care
Over the past few years, the Center for Accelerating Care Transformation (ACT Center) at Kaiser Permanente Washington Health Research Institute (KPWHRI) has worked with Vayu Health, a nonprofit startup in California, to design a program to support people who are living with diabetes that’s not well controlled. The Vayu program serves people who have insurance through Medicaid managed care plans and aims to help them achieve better diabetes control by providing whole-person care that addresses their medical, behavioral, and social needs.
Tapping into the ACT Center’s experience with program design and implementation, patient engagement and social health, KPWHRI Collaborative Scientist Kelsey Stefanik-Guizlo, MPH, is helping lead the ACT Center team that’s supporting Vayu in implementing and refining their program. She recently shared her thoughts on 2 early papers from the project — results from the initial pilot and a case study of the program implementation — and talked about what’s coming next as the program expands.
Why is this research important?
When diabetes is not well controlled, it can put people at risk for life-altering long-term complications, including heart disease, kidney disease, eye and vision problems, nerve damage, and more. Despite these risks, in 2021, 37.5% of people in California’s Medicaid program had a 3-month average of blood sugar control (known as an A1c) above 9%, which means their diabetes was not well controlled.
The reasons that people have a hard time controlling their blood sugar are varied and complex, and often include multiple contributing factors — such as having unmet medical, behavioral, and social needs. Health systems may be challenged to meet those needs for a lot of reasons. It can be difficult to match patients with the right type of care, and hard to get timely data on how well care is working. There’s a real opportunity to build a scalable and effective solution that can work across health care systems.
Our team at the ACT Center has been working with Vayu to create tools to support program implementation, such as an assessment to help Vayu determine if a clinic is ready to partner with them, a clinical staff training framework, and tools for tracking quality improvement data. Using data collected from interviews with Vayu staff and partners, we have also highlighted obstacles that might prevent the program from reaching its full potential — such as staff at participating clinics not being aware of the initiative or participants being reluctant to use the behavioral health services of the program.
How does the Vayu program work?
Vayu focuses on partnering with primary care providers at federally qualified health centers (FQHCs) to provide more support for individuals’ unmet medical, behavioral, and social needs. This support is provided by an integrated team that includes a community health worker, certified diabetes care and education specialist, behavioral health therapist, and registered nurse. The team is in frequent contact with program participants — monthly, weekly, or even daily, depending on the person’s needs. They work with participants to develop action plans based on the individual’s priorities, connect them to community resources, and support behavior changes to improve diabetes control.
The program prioritized hiring care team members who have lived experience that could help them build trust with participants. They were flexible about where people could receive care — in the clinic, virtually, and also in community spaces where participants felt comfortable. The focus of the program is whole-person care, so participants had support with things like learning to manage insulin injections and glucose monitoring, accessing resources for food assistance or transportation, or navigating the health care system or the pharmacy. Celebrating successes and building skills, knowledge, and confidence among participants were important elements of the program.
What were the main findings from the pilot study?
So far, Vayu has piloted its program at one federally qualified health center with 51 participants who had an A1c of over 9% in the last 6 months. Participants were enrolled for 12 months, and we tracked A1c values and assessed behavioral and social needs. There was also a comparison group of 477 patients who were not enrolled in the Vayu program.
From that pilot, we observed that Vayu enrollees had high levels of complex, unmet medical, behavioral, and social needs. For example, 83% of individuals had at least one behavioral health condition, such as depression, anxiety disorder, or substance use disorder. More than half of Vayu participants (51%) reported living with depression, a rate that is 4 to 5 times higher than that in the larger population of people with diabetes. More than half of participants also reported adverse childhood experiences, and more than 90% reported at least one unmet social need, such as insecurity around food, housing, or employment.
We found that the average monthly A1c among Vayu program participants was lower than that of the comparison group. When we began enrolling participants, A1c values were higher for Hispanic participants than non-Hispanic white participants. Over the 12 months of the pilot, that disparity declined and was no longer present at the end of the pilot. Vayu’s clinical team attributed these findings to their work to prioritize addressing participant-identified goals, building trust, and enhancing access to support to manage their diabetes and behavioral and social health needs.
What are the next steps for this research?
Vayu is now expanding its program by partnering with 2 additional FQHC clinics. They are aiming to enroll 150 to 200 people into the program across the clinics in 2024.
The ACT Center will be working with Vayu from now through most of 2025 to design and carry out a process evaluation. The team is excited to continue their collaboration with Vayu and to help them understand how the program is being implemented at the new clinics. As part of the evaluation, they will be talking with participants, Vayu clinical teams, and FQHC clinic staff and are looking forward to hearing their perspectives to inform the future of the program.
By Amelia Apfel
Drugs, diabetes, disparities
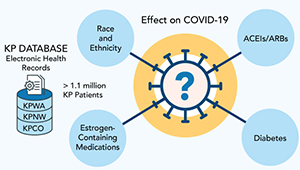
Studying COVID-19 risk and outcomes
Dr. Sascha Dublin tells how studies of KP electronic health record data can improve COVID-19 treatment and prevention.
SONNET study
Social risks: Do patients want health systems to help?
New research led by Leah Tuzzio, MPH, looks at patients’ unmet social risks and their desire for assistance.
healthy communities

Partnering with research, CRS program addresses social needs in primary care
Cindee DeWitt describes how Kaiser Permanente Washington’s community resource specialist program stands out among efforts to meet patients’ social needs.


