2024 Annual Report
Advancing health and well-being for all communities
Kaiser Permanente Washington Health Research Institute (KPWHRI) recently celebrated 40 years of impactful research. Over 4 decades, our discoveries have helped millions of people worldwide lead healthier, happier lives. We continued this work in 2024 with many notable findings. Among these:
- An innovative study found that a relatively simple intervention improved older adults’ blood pressure by encouraging them to sit less.
- One of KPWHRI’s many collaborations uncovered potential targets for future Alzheimer’s therapies by studying the disease on a cellular level.
- A large study found that integrating suicide care into primary care significantly reduced suicide attempts.
These findings, and all of the institute’s work in 2024, would not have been possible without our team of 258 dedicated scientists and staff.
Research highlights
In 2024, KPWHRI researchers contributed significant findings in many key areas of research, with 206 articles published in peer-reviewed journals. Much of our research also received attention from the media. Here are some of our research highlights in 2024:
Changing sitting habits shows meaningful impact
A KPWHRI study used a relatively simple approach — involving health coaching, an activity tracker, and a standing desk — to help older adults reduce sitting time by around 30 minutes a day. The reduction in sedentary time led to improvements in blood pressure comparable to those found in studies where participants increased their time spent exercising.
In the media: Decreasing sitting time 30 minutes reduces systolic blood pressure in older adults, Cardiology Advisor, May 1
Analysis supports new recommendation to begin mammogram screening at 40
KPWHRI researchers were part of a multi-site study that found breast cancer screening every 2 years beginning at age 40 has the potential to reduce death rates from the disease while minimizing screening harms, such as false-positive results. These findings informed the newly released U.S. Preventive Services Task Force breast cancer screening recommendations.
In the media: What kind and when is the right breast cancer screening for me? Kitsap Sun, July 20
Suicide attempts decreased after adding suicide care to primary care
After suicide care was integrated into routine primary care visits, KPWHRI researchers found a 25% decrease in the rate of suicide attempts in the 90 days following these visits. The study is the first to show that suicide risk screening in primary care, followed by safety planning, improved suicide prevention efforts in a health care setting.
In the media: Implementation of suicide care in primary care cuts rate of suicide attempts, Physician’s Weekly, Oct. 1
Mapping Alzheimer’s at the cellular level for new treatment targets
Researchers from the Allen Institute for Brain Science, UW Medicine, and KPWHRI have created the most detailed picture yet of how Alzheimer’s disease progresses at the cellular level. The study analyzed over 3.4 million cells from 84 donated brains, most from Kaiser Permanente Washington members in the Adult Changes in Thought Study (ACT Study).
In the media: Alzheimer’s research advances with Kaiser Permanente Partnership, KCPQ-TV Seattle, Oct. 23
When is Paxlovid right for COVID-19 treatment?
Paxlovid is recommended as a COVID-19 treatment for adults who are at high risk of severe complications. Thanks to a new predictive model, care teams and patients at Kaiser Permanente Washington can now use real-time data on individual risk factors and potential side effects to help guide their decision-making. The model was developed by KPWHRI’s Center for Accelerating Care Transformation (ACT Center).
Study sheds light on needs of young people with cancer
A KPWHRI study provided some of the most comprehensive information to date on potential care gaps for young cancer survivors. The study found that rates of emergency department use within 5 years of a cancer diagnosis were higher for those who had public insurance and were between 20 and 24 years old, female, and Black. Colorectal cancer and cervical cancer diagnoses were also associated with higher rates of emergency department use compared with other cancer diagnoses.
In the media: Emergency department use common among AYA cancer survivors, Cure, May 10
Bariatric surgery linked to lower risk of blood clots long-term
KPWHRI led the largest study to date exploring the long-term risk of blood clots in veins (venous thromboembolism) among adults with severe obesity who had weight-loss surgery. Patients who had surgery had a substantially lower risk of blood clots 1 and 5 years after their surgery than those who didn’t have the surgery.
In the media: Bariatric surgery-associated VTE risk decreases in long term, Medscape, June 17
Single question helps identify patients at higher risk of cannabis use disorder
A KPWHRI study evaluated the use of a screening tool in primary care settings that asks patients one question — how often they used cannabis in the last year. The responses can be used by clinical teams to help patients understand their risk of cannabis use disorder and to determine which patients might benefit from further screening.
Intervention supporting unhoused patients shows promise
Samaritan, a digital health intervention designed to assist individuals at risk for or experiencing homelessness, showed promising results in a pilot evaluated by KPWHRI’s Center for Community Health and Evaluation (CCHE). Notably, CCHE found that Samaritan benefited both the people experiencing homelessness who took part in the program as well as the health care system, which saw reduced costs.
More media highlights
KPWHRI’s research findings reached audiences nationwide through more than 50 news stories in 2024, including the select media mentions above. Here are some additional stories that made headlines:
- Nurses, access to medication expand treatment for opioid use disorder, Medscape, Dec. 19
- How vision loss and impairment could signal dementia: HealthLink, KING 5 News, Sept. 1
- How doctors can help demystify birth control amid online confusion, Science News, July 9Science News, July 9
- Managing depression in adults, JAMA Clinical Reviews podcast, June 10 podcast, June 10
- FDA approves new self-collection option for HPV testing, MedPage Today, May 15
- Surgery better for diabetes than medical, lifestyle changes, 4 systems find, Becker’s Hospital Review, Feb. 27
Finances
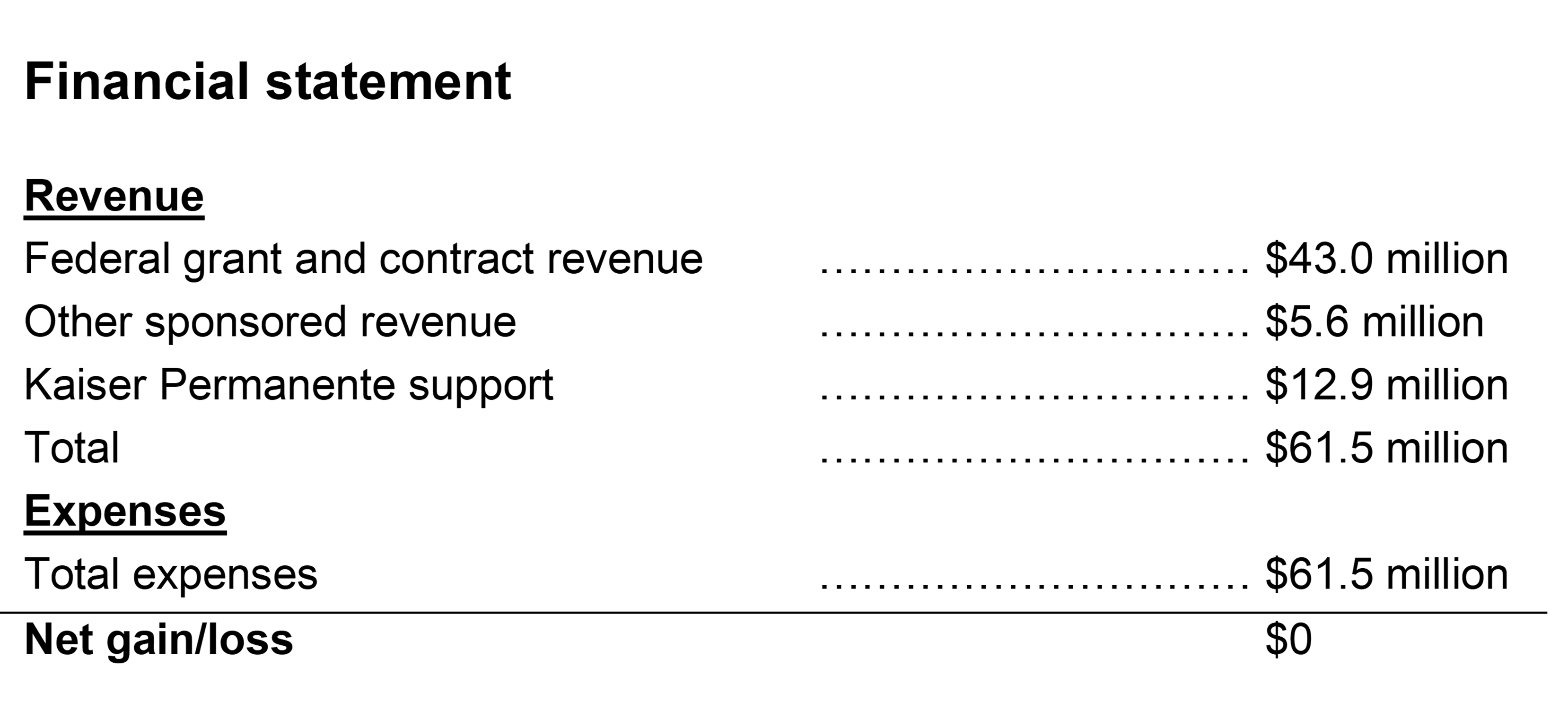
In 2024, KPWHRI’s operating budget was $61.5 million. Federal grant and contract revenue totaled $43 million and other sponsored revenue was $5.6 million. Our number of active grants stood at 280.
Download a PDF of the 2024 annual report.
KPWHRI's history

40+ years of research
Read about our history and watch a video celebrating our first 4 decades of impactful research.

We would like to extend a heartfelt thank you to our many collaborators, partners, participants, communities, and funders who make our research possible.
See KPWHRI’s website for more information on our research areas, capabilities, and latest news, and to subscribe to our newsletter.
Contact:
Bianca DiJulio
Senior Manager, Survey Research & Communications
bianca.s.dijulio@kp.org
1730 Minor Ave., Suite 1360
Seattle, WA 98101kpwashingtonresearch.org




