Start making sense: Taking Action on Overuse

MacColl Center’s Brian Austin and Michael Parchman are fans of the Talking Heads’ film, Stop Making Sense. But their latest project advises otherwise.
MacColl and Robert Wood Johnson Foundation help providers and patients hold hard conversations to curb habits of too much testing and treatment
An interview with Michael Parchman, MD, MPH, and Brian Austin: director and associate director, respectively, of MacColl Center for Health Care Innovation at Kaiser Permanente Washington Health Research Institute (KPWHRI).
How did you start the project called Taking Action on Overuse?
Parchman: Two years ago, the Robert Wood Johnson Foundation (RWJF) asked us to explore a troubling gap they saw between knowledge and practice: Efforts like Choosing Wisely were raising recognition that to improve quality, safety, and affordability, U.S. health care must quit overusing certain tests and treatments that do patients more harm than good. Yet providers, health care teams, and patients still seemed to struggle to engage in actually doing this work. Many organizations were trying, but each was building the road as they traveled, without a map.
Austin: In the first phase of the project, we spent a year studying best practices for reducing overuse. We reviewed the literature, including relevant behavioral economics, psychology, and sociology. We interviewed and did site visits with health care organizations, including our own, that have grappled with overuse. Gathering what works best, we developed an action-planning framework to guide the way providers and patients can do this work—with sense-making conversations among providers, health care teams, and patients at the framework’s heart.
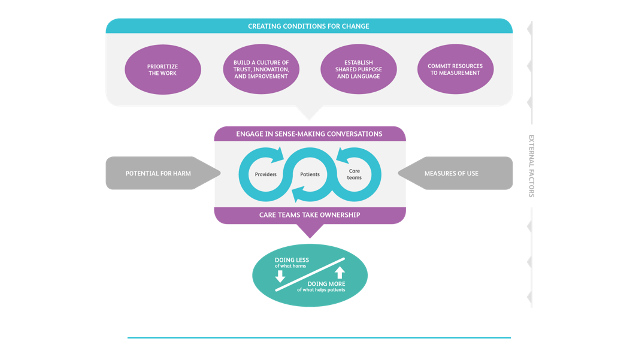
The Taking Action on Overuse conceptual framework for how to reduce low-value care.
Can you describe these conversations?
Parchman: Sure.Theidea is to encourageproviders and care teams to share how often individual team members order a test or treatment. Peer pressure works to change entrenched behavior. They also share anonymous stories with patients and with each other about the potential for harm: near misses, and patients who suffered harm from overuse.
We say: No data without stories, and no stories without data.
Parchman: We need to tell patients, “Let me tell you about someone who had this test done, and things didn’t turn out so well for them.”
Austin: To set the stage for these conversations, the framework advises: making this work a priority; building a culture of trust, innovation, and improvement; establishing a shared purpose and language; and committing resources to continuingly measuring use.
What’s happening now?
Parchman: We’re midway through the project’s second phase, helping three very different partnership sites use the action-planning framework to engage their providers:
At Swedish Medical Center in Seattle,we’re engaging providers, teams, patients, and their families to use care planning to reduce overuse of hospital stays and emergency visits for patients with multiple chronic diseases.
At UCLA Health in Los Angeles, we’re engaging gastroenterologists and referring providers not to overuse upper-GI endoscopy for gastroesophageal reflux. Doing less of this potentially harmful screening may give gastroenterologists more time to do helpful screening for colorectal cancer.
And at Missouri Primary Care Association, we’re tackling overuse of long-term opioids for chronic pain at a large network of community health centers.This topic is near and dear to my heart.
Austin: We’re supporting each site with a clinical champion internal to the site, a project manager at that site to help the clinical champion, an external quality improvement coach, and a MacColl staffer as a liaison.
How is it going?
Parchman: We’re pleased with our progress, even though this has been a challenging project. We physicians are the most cautious and careful people you’d ever want to meet. That’s part of the reason for overuse—in addition to the U.S. health care system’s perverse financial incentives to do more.
Austin: The teamwork on the project is rewarding. We’ve assembled an interdisciplinary team—and given them chances to stretch and take on new facets of work. Our coaches are Connie Davis, Mike Hindmarsh, and Kathleen Reims. (Connie and Mike worked at MacColl for years.) Nora Henrikson, Lorella Palazzo, and I are the MacColl liaisons.
Parchman: Other great team members include Paula Blasi, Diana Buist, Diana Charbonneau, Dona Cutsogeorge, Gabrielle Gundersen, Leslie Jauregui, and Nicole Van Borkulo. And our RWJF project officer, Emmy Ganos, is an equal partner: Overuse was her PhD dissertation topic!
What’s next?
Parchman: We’re planning a big-tent meeting in about a year to train coaches, trainers, and quality improvement experts in the framework, which we’ll have tested. Then these pollinators will go forth and spread the work to other organizations.
Austin: So far we hear the work we’re doing jibes with and advances other work on overuse nationally—but doesn’t duplicate it.
Parchman: Most of the Choosing Wisely work has been low-hanging fruit like antibiotics for upper respiratory infections and MRIs for back pain. But U.S. health care hasn’t even started to tackle massive overuse of some big-ticket tests and treatments. We’ve barely scratched the surface of the opportunities to do this work.
How can people learn more about Taking Action on Overuse?
Austin: Our new website has the results of our research so far, and we’ll update it. You can take the self-assessment, get the action-planning framework and change package, and give us feedback for improvement.
Read about our interactive hands-on workshop at the 2017 Lown Institute conference.
Watch the April 2017 webinar presented by Choosing Wisely Canada, featuring Dr. Michael Parchman: The Taking Action on Overuse Framework and Change Package for Reducing Low-Value Care
RWJF grant 72546 supports this project.
by Rebecca Hughes
Co-Researchers
Paula R. Blasi, MPH
Senior Collaborative Scientist
Nora Henrikson, PhD, MPH
Associate Investigator
Lorella Palazzo, PhD
Senior Collaborative Scientist
Low-Value Care

Stop! In the name of health—lessening low-value care
MacColl engages teams to ‘de-implement’ needless tests and treatments, doing less overused low-value care that might harm patients.



