Addictions
Scientists at Kaiser Permanente Washington Health Research Institute (KPWHRI) conduct innovative research to help patients and their care teams prevent and treat problems caused by use of alcohol, cannabis, opioids, and other drugs.
For more than 3 decades, KPWHRI researchers have focused on improving how health systems measure and address alcohol and drug use in nonjudgmental, patient-centered ways, as part of whole-person health. This has resulted in innovations in care and practical tools for patients. For example, KPWHRI’s alcohol-related research has led to resources — including a patient decision aid and video — that help overcome stigma so that patients and families can find the help they want and need.
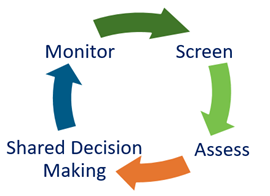
KPWHRI researchers also conduct studies to improve screening for substance use and how this is documented in the electronic health record, including for both medical and nonmedical cannabis use. Another focus is ensuring that evidence-based treatments for alcohol and drug use are accessible to the patients who may benefit from them.
Research highlights
 Adding alcohol-related care to primary care
Adding alcohol-related care to primary care
A KPWHRI study found that a novel approach to integrating alcohol-related care into primary care increased annual alcohol screening and preventive counseling. The study — called the Sustained Patient-Centered Alcohol-Related Care (SPARC) trial — also demonstrated an adaptable approach for integrating behavioral health care into primary care. To assist other health systems and researchers, the study team has shared tools and resources for behavioral health integration on the SPARC website.
 Gleaning insights on cannabis use
Gleaning insights on cannabis use
Washington was one of the first states to legalize recreational cannabis use in 2012. As a result, Kaiser Permanente Washington researchers are uniquely positioned to study the impact of cannabis use on patients' lives and health. KPWHRI research suggests that 1 in 5 people who use cannabis daily are at risk for moderate to severe cannabis use disorder. However, the risk may be lower with medical cannabis use than recreational use.
 Improving support for opioid use disorder treatment
Improving support for opioid use disorder treatment
Most people with opioid use disorder never receive medication treatment, even though it is effective (and potentially life saving) and can be provided in primary care. A trial led by KPWHRI researchers found that more people received treatment for opioid use disorder when nurse care managers were added to primary care teams to provide support for ongoing treatment.
 Effectively managing pain without opioids
Effectively managing pain without opioids
KPWHRI's Center for Accelerating Care Transformation (ACT Center) created the Integrated Pain Management (IPM) Program to provide safe alternatives to opioids for people with persistent (chronic) pain. The researchers worked with patients, care teams, and leaders at Kaiser Permanente Washington to design, implement, and evaluate a primary care-based pain management program. The IPM team also worked closely with patient partners to produce the Toolkit for Managing Persistent Pain, which offers support and resources for people with chronic pain.
 Better tools for assessing substance use disorder
Better tools for assessing substance use disorder
Working with clinical partners, KPWHRI researchers developed an 11-item checklist to measure potential symptoms of substance use disorder. Clinicians then began using the checklist as a tool in primary care. A study confirmed the value of the checklist, finding that it did well at providing information on the presence and severity of substance use disorder. Of particular note: The checklist performed well among people of different ages, races, sexes, and ethnicities.
Researchers in Addictions
 Julie Angerhofer, PhD, MPHAssociate Investigator |
 Jennifer F. Bobb, PhDSenior Biostatistics Investigator |
 Katharine A. Bradley, MD, MPHSenior Investigator |
 Clarissa Hsu, PhDAssociate Investigator |
 Noorie Hyun, PhDAssociate Biostatistics Investigator |
 Morgan Justice, MASenior Collaborative Scientist |
 Gwen Lapham, PhD, MPH, MSWAssociate Investigator |
 Theresa E. Matson, PhD, MPHCollaborative Scientist |
 Jess Mogk, MPHCollaborative Scientist |
 Yu-Ru Su, PhDAssociate Biostatistics Investigator |
 Paige D. Wartko, PhD, MPHSenior Collaborative Scientist |
AFFLIATE RESEARCHERS
Kevin Hallgren, PhD
Associate Professor
Department of Psychiatry and Behavioral Sciences
University of Washington
Emily Williams, PhD, MPH
Investigator
Health Services Research & Development
VA Puget Sound Health Care System
Edwin Wong, PhD
Associate Professor
Department of Health Services and Population Health
University of Washington



