Of big data, systems change, research partnerships, and planting redwoods

A conversation with KPWHRI’s Michael Von Korff, ScD, as he retires after 36 years of transformative health research
Q. When people retire, they’re often asked to reminisce. But I know you’d rather talk about what’s ahead. Do you have any advice for us?
I do. You need to keep in mind that science is organized learning. And we’re at the point in American health care where we can no longer study change only by conventional randomized trials, although they remain essential.
We’re working in complex systems, where a lot of things need to change all at once. So it is insufficient to ask only, “What good does patient education do?” Or, “What good do guidelines, reminders, or care managers do?” All of these are separate components that may only be truly effective when implemented in tandem. You have to look at whole systems. It’s difficult to randomize changes in entire health care systems—not practical.
So I think it’s great that the Institute is trying out new research paradigms. If a health care organization is making consequential changes, then you need to compare it to other settings that haven’t made those changes. Controlled comparisons are the essence of both the scientific method and of learning health systems.
Q. In the past, we often did studies by introducing changes for one set of patients and not others, or sometimes for one set of clinics but not other. Then we would compare the results. Are you saying that won’t work anymore?
Right. Now we tend to change things at all clinics at once because of our information systems and the need for standardization across clinics. So, if you limit your research to Kaiser Permanente Washington, you don’t have an adequate control. That makes it hard to evaluate big system changes.
To have a robust learning health system, we need to have working relationships with other large health systems. We can’t be looking only at Kaiser Permanente Washington. We need collaborative relationships and access to data from other places for comparison. The work Greg Simon is doing right now with the Mental Health Research Network is a great example, and Lynn DeBar’s research on improving care for chronic back pain in the NIH Collaboratory is another. It is cool that KPWHRI is setting the pace for this kind of research. The Institute’s best work is yet to come.
Q. Then the “population laboratory” of the future includes eight Kaiser Permanente regions, plus other health systems, right?
Exactly. If we want to realize our potential, we need to focus on collaboration. For example, Kai Yeung is starting to work with the Washington All-Payer Claims Database. In the future, that may allow us to compare care within Kaiser Permanente Washington to other health care organizations in Washington state.
One of our highest priorities should be building access to external comparator data, collaborating with researchers from other settings, and getting good at using big data from multiple large health care organizations to learn what works and what doesn’t. Fortunately, we already have enormous strengths for this kind of research.
Q. What about the studies where we roll out changes sequentially within our own system, introducing them to one clinic after another and then comparing results?
That’s called a stepped-wedge design. I am not a fan. It often takes too long to make changes—and then there isn’t time to develop enough experience to make reliable comparisons. The evaluation that we recently did of opioid risk reduction at Kaiser Permanente compared patients in our integrated group practice with those in our external network over a nine-year period. We learned a lot, but when it came to comparing overdose rates, the network had only one-third the number of patients as the integrated group practice, so our results were inconclusive. There was a significant reduction in overdose rates within the large group practice patient population, but the comparison of overdose rate reduction to the smaller network patient population was nonsignificant. The stepped-wedge design often compares much smaller patient populations for relatively short time periods.
Q. So we need controls that are just as big as Kaiser Permanente Washington?
Yeah, or larger. We’re headed in that direction, but this needs to be a strategic imperative. Until now, we’ve been opportunistic, doing what we’re funded by others to do. But I think this needs to be an Institute-wide priority for the future, not dependent only on external funding.
Q. What other advice do you have?
From the very beginning we have done well because we give things away. We give away our ideas and our expertise. We share our data. We give people credit. We are very collaborative. Ed Wagner instilled that, and we followed his example. This has helped us build relationships of trust with people at other institutions. Learning to build trust and goodwill with colleagues from other organizations is among the most important skills a young researcher can develop. It also helps if you’re fun to work with.
Q. Well, you’ve always had a reputation for that.
Well, I tried. I always felt I owed a debt to the Institute’s staff for being so dedicated and creative in developing the systems and capabilities that made it easy to do our research.
Q. So while the rest of us are buried in grants, contracts, and IRB applications, what are you going to be doing?
My partner Linda, our son Douglas, and his partner Cory will be planting trees and growing cranberries and bamboo on the South Coast of Oregon. We’ve got 80 acres, largely timber plus five acres of cranberries and one acre of bamboo. Planting trees is very satisfying because you know they will be growing for hundreds of years. The coastal redwoods I just planted live for up to 2,000 years. I planted 400 trees this year and I’m aiming to plant 600 next year.
Q. Sounds intense.
Well, as Monty Python used to say, “And now for something completely different!” But we’re keeping our place in Seattle. And I will keep in touch with my friends here. I plan to hang around to help others with their research if they want. That is more fun for me than should be legal.
Q. Let’s stay in touch!
OK!
To learn more about the April 23 seminar honoring Dr. Michael Von Korff, please visit our events page.
—by Joan DeClaire
opioid research
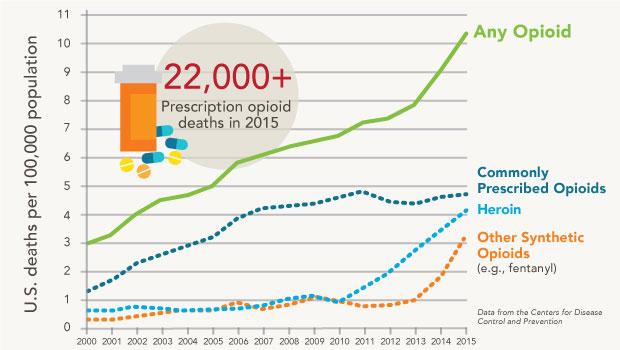
Stopping the opioid epidemic: Priority research at KPWHRI
Opioid misuse and overdose are now a national priority. For decades, KPWHRI has worked to help patients find safe, effective ways to manage chronic pain.
Learn more about our work in opioid research.
one scientist's legacy

Celebrating 36 years of research to improve care for depression and chronic pain
Dr. Michael Von Korff, one of KPWHRI’s founding scientists, has helped to make people healthier around the world, improving how care is provided.
study of opioid use

Long-term opioid risks are the focus of $10 million KPWHRI study
Dr. Denise Boudreau launches a collaborative project with Kaiser and other health systems on the safety of long-term prescription opioid use.
looking ahead

Tackling opioids: Rethinking pain management
Kaiser Permanente Washington can use its expertise in non-drug pain management to advance alternatives to the "medicalized" approach.
partnerships

Think globally, act locally: KPWHRI helps improve care with the Bree Collaborative
KPWHRI investigators contribute time, knowledge, and expertise to better care in Washington State around opioid prescribing, chronic pain, and more.


