Diabetes is more common among minorities at lower weights

At normal weight, Pacific Islanders are 3 times likelier than whites to have diabetes, Kaiser Permanente research finds
SEATTLE, September 19, 2019—Being overweight or obese is commonly linked to diabetes, but a new Kaiser Permanente study finds the connection differs widely by race and ethnicity. Members of racial and ethnic minority groups were much more likely to have diabetes or prediabetes at lower weights—even at normal or below-normal body mass index (BMI)—according to research published in Diabetes Care: “Racial/Ethnic Disparities in the Prevalence of Diabetes and Prediabetes by BMI: Patient Outcomes Research To Advance Learning (PORTAL) Multisite Cohort of Adults in the U.S.”
The large analysis included more than 4.9 million people of diverse backgrounds and geographies who were part of the nationwide Patient Outcomes Research to Advance Learning network. The PORTAL study group, supported by the Patient-Centered Outcomes Research Institute, includes data on more than 12 million patients contributed by all regions of Kaiser Permanente, along with HealthPartners in Minnesota and Denver Health.
Normal-weight Hawaiians and Pacific Islanders were 3 times more likely to have diabetes than normal-weight white people. Diabetes prevalence at normal BMI was 18 percent for Hawaiians/Pacific Islanders versus just 5 percent for whites; prevalence was also high for blacks (13.5 percent), Hispanics (12.9 percent), Asians (10.1 percent), and American Indians/Alaskan Natives (9.6 percent).
Disparities were also found in prediabetes but were not as pronounced. Results also differed by sex. Asians, Hispanics, and Hawaiians/Pacific Islanders had a higher prevalence of prediabetes at lower BMIs than other groups, particularly among women.
“This study suggests that minorities need careful screening for type 2 diabetes and prediabetes, even at body weights that are considered normal,” says coauthor David Arterburn, MD, MPH, a senior researcher at Kaiser Permanente Washington Health Research Institute in Seattle. “Failure to screen minority patients early could lead to further disparities in downstream health outcomes. So these data should be a call to action for primary care providers.”
For primary care clinicians, the findings could signal a change in how they screen racial and ethnic minority patients for diabetes and prediabetes, says senior author Assiamira Ferrara, MD, PhD, a senior research scientist with the Kaiser Permanente Division of Research in Oakland. “This study suggests that along with screening patients who are overweight and obese, minorities should probably be screened even if they have a normal BMI, particularly as they get older,” Dr. Ferrara says.
Conclusions about understudied groups
This study is one of the largest that has examined the relationship between BMI and diabetes and prediabetes prevalence. The study also included large enough samples of some understudied minority groups to draw conclusions about them. The study offers new information about diabetes prevalence across BMI categories among Asians, Hawaiians, Pacific Islanders, American Indians, and Alaskan Natives across the country.
This study took into account neighborhood-level measures of income and education, neither of which were found to fully explain the racial/ethnic differences in prevalence of diabetes beyond BMI. While access to primary care is a major factor in health care disparities, it was not seen as a contributor in this study, because all the patients had health insurance and were members of integrated health systems.
The authors speculated that people of varying races and ethnicities could have physiological differences relating to diabetes, citing the example of Asians having a higher share of body fat and visceral fat at the same BMI as other groups, which could lead to insulin resistance, prediabetes, and diabetes.
Lead author Yeyi Zhu, PhD, a research scientist with the Kaiser Permanente Division of Research, calls for better understanding of how the physiological mechanisms of diabetes may vary. “Future research could focus on body composition, genetics, and other lifestyle factors that may contribute to disparities in chronic disease burden,” she says.
Dr. Zhu also notes that the analysis identified a group of people at risk who don’t get as much attention for diabetes risk: those who are underweight. The study found significant differences in diabetes prevalence among underweight men, ranging from 7.3 percent in whites to 16.8 percent in American Indians/Alaskan Natives.
The study was funded by grants from the Patient-Centered Outcomes Research Institute and the National Institutes of Health.
Authors also include Deborah Young, PhD; Margo A. Sidell, ScD, MSPH; and Corinna Koebnick, MSc, PhD, of the Kaiser Permanente Southern California Department of Research and Evaluation; Matthew F. Daley, MD, of the Kaiser Permanente Colorado Institute for Health Research; Jay Desai, PhD, of HealthPartners Institute in Bloomington, Minnesota; Stephanie L. Fitzpatrick, PhD, of the Kaiser Permanente Northwest Center for Health Research in Portland, Oregon; Michael A. Horberg, MD, of the Kaiser Permanente Mid-Atlantic Permanente Research Institute; Emily McCormick, MPH, of the Denver Public Health Department; and Caryn Oshiro, PhD, of the Kaiser Permanente Hawaii Center for Health Research.
Diabetes is an active area of study for Kaiser Permanente Research.
About Kaiser Permanente Washington Health Research Institute
Kaiser Permanente Washington Health Research Institute (KPWHRI) improves the health and health care of Kaiser Permanente members and the public. The institute has conducted nonproprietary public-interest research on preventing, diagnosing, and treating major health problems since 1983. Government and private research grants provide our main funding. Follow KPWHRI research on Twitter, Facebook, and LinkedIn, or subscribe to our free monthly newsletter.
About Kaiser Permanente
Kaiser Permanente is committed to helping shape the future of health care. We are recognized as one of America’s leading health care providers and not-for-profit health plans. Founded in 1945, Kaiser Permanente has a mission to provide high-quality, affordable health care services and to improve the health of our members and the communities we serve. We currently serve more than 12.4 million members in eight states and the District of Columbia. Care for members and patients is focused on their total health and guided by their personal Permanente Medical Group physicians, specialists and team of caregivers. Our expert and caring medical teams are empowered and supported by industry-leading technology advances and tools for health promotion, disease prevention, state-of-the-art care delivery and world-class chronic disease management. Kaiser Permanente is dedicated to care innovations, clinical research, health education and the support of community health. For more information, go to: kp.org/share.
news release

Weight-loss surgery linked to fewer diabetes complications
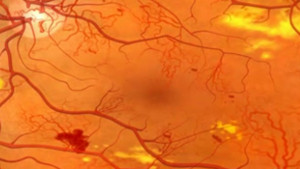
Large, long-term study finds half as much nerve, kidney, and eye disease after bariatric surgery than with usual carehealthy findings blog
Bariatric surgery may have ‘legacy effect’ on diabetes complications
Dr. Arterburn linked even short-term diabetes remission to less risk for microvascular kidney, eye, and limb diseases



