When is Paxlovid right for COVID-19 treatment?

New risk model uses advanced analytics to guide informed treatment decisions at Kaiser Permanente Washington
Even if you aren’t familiar with the latest prescription treatments for COVID-19, the name “Paxlovid” probably rings a bell. Initially authorized for emergency use by the Food and Drug Administration (FDA) in late 2021, Paxlovid is now approved for treating COVID-19 in adults who are at high risk of severe complications, such as hospitalization or death.
The FDA provides basic guidelines for prescribing Paxlovid, but it’s up to health care providers to assess a patient’s level of risk — and to weigh that risk alongside the potential side effects, such as loss of taste, diarrhea, and nausea, and certain medication interactions that can be life-threatening. How do health care organizations, care teams, and individual patients decide when Paxlovid is the right choice for COVID-19 treatment and ensure that it’s prescribed to those who are most likely to benefit?
Thanks to a new predictive model, care teams and patients at Kaiser Permanente Washington can now use real-time data on individual risk factors to help guide their decision-making. The model was developed by the Center for Accelerating Care Transformation (ACT Center), which is part of Kaiser Permanente Washington Health Research Institute (KPWHRI).
Partnering to develop an evidence-based way to inform treatment decisions
In early 2023, the ACT Center’s clinical partners on Kaiser Permanente Washington’s Communicable Disease Ambulatory Therapy (CDAT) team asked for help identifying patients at high risk of being hospitalized after COVID-19 infection. Clinical guidelines already recommend Paxlovid for people age 65 and older and for those with weakened immune systems. But the CDAT team wanted to understand individual risk levels for patients age 50 to 64, so that they could offer more information and guidance about whether the potential benefits of Paxlovid would outweigh the risks of taking it.
“Earlier in the pandemic, our guidelines on the use of Paxlovid were relatively simple. We treated everyone over the age of 65, as well as individuals who either had clinical conditions that impacted their immune systems or who were on medications that did the same,” explained Tolani Mwatha, MD, Kaiser Permanente Washington’s associate medical director for Primary Care and medical director of operations for Communicable Diseases.
“As we got further into the pandemic, we started wondering if we were missing patients in the 50-to-64-year range who had a higher risk of complicated disease. The Centers for Disease Control and Prevention (CDC) also started recommending that Paxlovid treatment be considered for all patients over age 50. But there weren’t any good guidelines on how to make treatment decisions in that age group. We had the opportunity to partner with the ACT Center to solve that question.”
Creating a risk model that’s both rigorous and flexible
Leveraging their expertise in risk prediction model development and implementation, the ACT Center’s advanced analytics team collaborated with CDAT to develop, validate, and implement a model that predicted an individual patient’s risk of hospitalization with COVID-19. The goal was to create a model that accurately reflects Kaiser Permanente Washington’s population of patients age 50 to 64 — and to implement the model where CDAT providers could easily access it.
The team started with a predictive model created at Kaiser Permanente Colorado for patients age 65 and older and then adapted it to incorporate several new variables that were indicated as potential predictors of higher risk for hospitalization from COVID-19 — for example, a diagnosis of chronic kidney disease or a prescription for immune-suppressive medications. The team also made the important decision to include race as a variable in the model to account for the fact that white non-Hispanic patients are at lower risk of being hospitalized due to COVID-19.
“When developing this model, we had the opportunity to ensure its use would improve access to COVID-19 treatment for patients from racial and ethnic groups that have traditionally experienced disparities in care,” said Yates Coley, PhD, an associate biostatistics investigator at KPWHRI who leads the ACT Center’s predictive analytics work. “There have been numerous examples of clinical prediction models that have exacerbated health disparities by ignoring existing inequities, so we were proactive in designing a tool that would support more equitable COVID-19 care.”
The final step was to implement the validated risk model in Epic — Kaiser Permanente’s electronic health record — where it would be at providers’ fingertips during encounters with patients recently diagnosed with COVID-19. One benefit of the model is that the risk score can be recalculated based on information gathered during the visit. For example, a provider can add information about the patient’s health status (such as a recent diagnosis or vaccination) and recalculate the score to ensure the latest information is incorporated.
“The CDAT team has unique challenges in caring for patients with COVID-19. The clinicians see patients with whom they don’t have an established relationship and who are sometimes new to Kaiser Permanente. Their clinician is learning about them and assessing their risk, often in less than 15 minutes,” said Kristine Rogers, MS, a lead systems administrator at KPWHRI and the ACT Center’s resident expert on implementing risk models in Epic.
“Our predictive model needed to be responsive enough to not just produce a risk score for a patient on demand — but to recalculate it as needed if the clinician learned something about the patient that would affect their risk.”
What the new model means for care teams and patients
In August 2023, the CDAT team started using the new risk model in Epic during visits with patients age 50 to 64 who had a new COVID-19 diagnosis. The model uses data from the patient’s history and the current visit to identify those who are at high risk of hospitalization or death from COVID-19 and who wouldn’t otherwise be flagged for Paxlovid treatment based on existing clinical criteria.
“The ACT Center developed an elegant COVID-19 risk tool that we currently use across several clinical teams in Kaiser Permanente Washington to guide treatment decisions,” said Mwatha. “This tool allows a provider to assess an individual’s risk of developing complications from COVID-19 and thus make better decisions on who would benefit the most from Paxlovid.”
CDAT provider Sherri Giragosian, PA-C, highlighted another benefit of the tool: supporting shared decision-making. “The risk model developed by our ACT Center’s advanced analytics team has enabled me to have solid data to share with patients who aren't sure whether they need Paxlovid. It provides me with a tool to help in the shared decision-making process, especially for our patients who are 50 to 64 years old. I am grateful to the team for designing it in such a short time after the CDC announced that people over 50 years old should consider Paxlovid.”
Added Mwatha: “We now have an efficient and useful tool that helps us answer an important question about treating a new disease. It was incredibly exciting to work in collaboration with research scientists to harness the power of data and improve day-to-day care for our members.”
Many thanks to our clinical partners at Kaiser Permanente Washington and the ACT Center team members who made this work possible: David Arterburn, Yates Coley, Barbara Detering, Chase Ford, Robert Frazier, Sharon Fuller, Sherri Giragosian, Dan Kent, Purple Pearl Lawson, Sarah Levy, Sophia Mun, Tolani Mwatha, Roy Pardee, Ryan Peterson, Annie Piccorelli, Carol Rappaport, Kristine Rogers, Alyce Sutko, Paul Thottingal, Emily Westbrook, Benjamen Wilson, and Amy Zern.
By Jessica Ridpath
This was adapted from a story originally published by the ACT Center.
Visit the ACT Center

Moving research into action, together
KPWHRI’s Center for Accelerating Care Transformation improves health for people and communities by streamlining the path from research to practice.
Healthy findings blog

What motivates Yates Coley’s work on prediction models?
Their work contributes to improved quality of care and better understanding of patients’ needs.
From research to practice
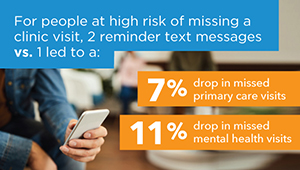
Predicting and preventing missed clinic visits
Biostatistician Yates Coley reports on new predictive analytics work that’s decreasing missed visits at KP Washington.
COVID-19 treatments

New report supports value of COVID-19 drugs
A team led by KPWHRI's Kai Yeung, PharmD, PhD, reviewed trial results for cost-effectiveness of 3 treatments.
INNOVATIONS IN CARE

Helping KP Washington lead in intelligent health care
How our Learning Health System Program is using statistical methods and machine learning to respond to COVID-19.



