Behavioral health team wins 2016 Birnbaum award
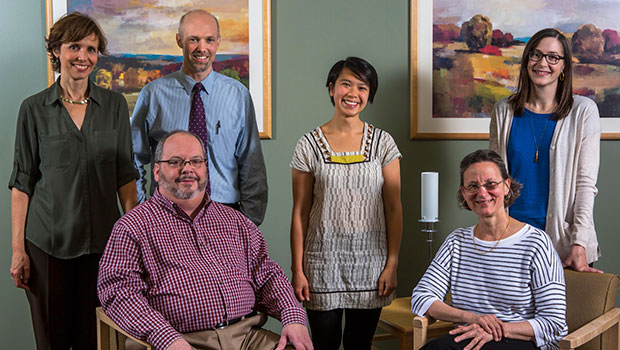
Photo caption: Behavioral Health Integration clinical and research team members. Left to right, back: Paula Lozano, MD, MPH; Ryan Caldeiro, MD; Amy Lee, MPH; Rebecca Parrish, LICSW. Front: Larry Marx, MD; and Katharine Bradley, MD, MPH.
Patients benefit when behavioral health and substance use screening are part of primary care. A Group Health team was honored for this care improvement.
Each year, Group Health Research Institute (GHRI) presents the Birnbaum Award to Group Health staff members whose collaboration in research has significantly improved patient care. The 2016 award honored the clinical team that is working with GHRI researchers on Group Health’s Behavioral Health Integration (BHI) initiative. The goal of BHI is to improve access, reliability, and quality of care for patients with mental health and substance use concerns by routinely addressing these issues in primary care. BHI was piloted in three Puget Sound area clinics, and was so successful that in January 2016 Group Health leadership approved extending it to all 25 primary care locations.
Ideally, a person’s primary care provider has a thorough understanding of their overall health and will identify behavioral health conditions, engage in shared decision making about treatment options, and provide support in accessing care, including referrals to specialists when necessary. But all too often, unhealthy alcohol or drug use, depression, or anxiety have gone unrecognized—and therefore untreated—unless the patient experiences a crisis or initiates a discussion with their provider. BHI embeds an evidence-based screening questionnaire into the standard work of primary care. If the results indicate a need for further assessment or intervention, social workers engage as part of the primary care team to help develop a treatment plan.
How BHI can save lives
Social worker Kara Rice shared this story about the power of BHI:
A 24-year-old patient had come into the clinic to be seen for a cold. Because of the BHI screening standards, we were alerted to the fact that he wasn’t just suffering from a cold—he was acutely suicidal. I was paged to come talk with him and learned that he was not only severely depressed, he had attempted suicide twice in the past two weeks.
I completed a suicide risk assessment with him, and he screened very high. We talked about his immediate safety, and I discovered that he had limited outside supports. Because his safety couldn’t be guaranteed if he went home, we talked about inpatient psychiatric treatment, which he agreed was a good idea.
I asked his primary care doctor to place lab orders and then walked the patient to Urgent Care, where they were happy to monitor him until a bed became available. Then I coordinated his follow-up care. The patient was authorized for psychiatric admission within four hours. I also talked with his parents, who waited with him in Urgent Care and later drove him to his psychiatric placement.
Thanks to BHI, we had systems in place that let us know this young man was in immediate danger, and we were able to intervene and help him right away. Who knows what might have happened if he had come and gone and been treated only for his cold?
Success from collaboration and conversations
The success of the BHI initiative is the result of close collaboration among administrators, staff, and providers at the three pilot clinics and dozens of Group Health staff members in multiple departments, including Behavioral Health Services, Care Delivery Information Technology, and the Clinical Improvement and Prevention team. Financial support has been equally diverse. The Agency for Healthcare Research and Quality, the GHRI Development Fund, the Group Health Foundation Partnership for Innovation, and the National Institute on Drug Abuse have each provided funding for different aspects of the program.
“We’ve heard from patients that they appreciate having their behavioral health concerns addressed in primary care,” says GHRI Senior Investigator Katharine Bradley, MD, MPH, who nominated the BHI team for the Birnbaum Award. “This integrated approach to care has made a big difference in their lives.”
Larry Marx, MD, medical and operations director of behavioral health, agreed. “This work is a highly successful collaboration between Behavioral Health, GHRI, and the primary care teams. The patient stories reflect the importance of the work: the need for health care systems to destigmatize mental health and substance use concerns by proactively screening, assessing and, most importantly, having a conversation with our patients about how to best help them address these issues.”
by Janet Hendrickson, MS
The 2016 Birnbaum Award winners
Behavioral Health Support Services
- Larry Marx, MD
- Ryan Caldeiro, MD
- Janet Boltwood, LICSW
- Leslie Gilbert, LICSW
- Tory Gildred, LICSW
- Kate Lee
- Rebecca Parrish, LICSW
- Carolyn Rue
Olympia Medical Center
- Noah Ceazan, MD
- Kari Fye, RN
- Sandra McLauchlin
- Peter Mendy, RN
- Mithila Pathare, LICSW
- Linda Phan
- Kristalene Pitts-Palmerton, LICSW
- Kara Rice, LICSW
- Renee Santos, RN
- Amber Skrivanich
- Julia Sokoloff, MD
- Angela Sparks, MD
- Lisa Spatz, MD
Everett Medical Center
- Jennifer Bolnick, MD
- Estee Carton-Bozzi, LICSW
- Valentina Denisiuk, RN
- Megan Gary, MD
- Janet Gifford
- Nancy Marriott
- Claire Neal, RN
- Eugene Ocampo, MD
- Ana Paiva, PA-C
- Heidi Sitton, RN
Northgate Medical Center
- Kristin Conn, MD
- Sallie Dacey, MD
- Michelle Donahue, RN
- Georgette Fallgatter, RN
- Angela Garza McWethy, LICSW
- Andrew Jacobson, MD
- Michelle Ortega
- Cheryl Paradise
- Lisa Sumerwell, RN
- Santino Telles
- Sandra Welch, RN
Clinical Improvement & Prevention
- Maria Cardenas-Anson
- Avra Cohen, RN
- Robyn Mayfield
- Susan McDonald, RN
- Kristine Moore, RN
- Kimberly Wicklund
Care Delivery Information Technology
- Fred Brodsky, MD
- Woody Favinger
- Sarah Miller
- Ryan Peterson

Group Health Research News July 2016
In this issue
- Behavioral health team wins 2016 Birnbaum award
- CCHE mourns the passing of founding director Bill Beery
- Dr. Leana Wen: Better care is not our biggest health challenge
- Don’t wait: Dr. Leana Wen urges public health action now
- From war to Group Health: The journey of Stefan Golston
- Big data plus real-world context equals community health improvements
- The 1 percent’s longevity: income is not the only inequality



