3 concrete steps to lessen disparities in health care

Latinos are underrepresented in U.S. research studies. Magaly Ramirez, PhD, explains how to achieve greater diversity
By Magaly (Maggie) Ramirez, PhD, MS, a CATALYsT scholar at Kaiser Permanente Washington Health Research Institute (KPWHRI) and assistant professor of Health Services at the University of Washington School of Public Health
Medical researchers nationwide are stepping up their efforts to address the growing inequities in health and health care. Such change demands rethinking how we do our work. To eliminate the systemic racism in our health care system, we must achieve greater diversity in our research.
Last month, at the Adult Changes in Thought (ACT study) research symposium, I was invited to speak on the types of discrimination that compromise many studies and the measures we can take to end such practices. My research focuses on the role that information technology can play to close racial and ethnic gaps in health. Most recently, as a CATALyST scholar at KPWHRI, I have been investigating how technology can improve support for Latino caregivers of Latino people with Alzheimer’s disease and related dementias.
Latinos are at least 50% more likely than non-Latino whites to develop dementia. Yet while Latinos make up 17% of the U.S. population, they represent 1 percent of participants in National Institute of Health (NIH) trials. How can we do better at engaging Latinos and, more generally, people of color in research? There are 3 actions I recommend, drawing from my own research experience.
First, stop excluding people from participating in research if they aren't fluent English speakers. Eight percent of the US population has limited English proficiency, with Latinos comprising a large majority of that group. Research grants need to set aside funds for creating study materials in multiple languages. A great example is the NIH-funded stroke prevention study that I worked on in graduate school: It had materials in English, Spanish, Mandarin, Cantonese, and Korean. Inclusion was a priority for these investigators.
The second action is to create more diverse research teams. Latinos, for instance, account for only 3.5% of principal investigators supported by NIH funding. Researchers of color are more likely to focus their research on people of color. In turn, they may be better positioned to gain the trust of these communities. There's evidence that people of color are more likely to participate in research if they're recruited by staff they can identify with. In my CATALyST research on Latino caregivers, we have a tiny team: me and a staff member. I'm a bilingual, bicultural Latina, a first-generation American, and my staff member is a recent Mexican immigrant who worked as a physician serving marginalized communities in Mexico. We understand the cultural idioms, the metaphors, the sayings, the humor, the customs that are part of our speech, and our culture. We believe that this helps participants to feel comfortable and share their perspectives more freely.
Third, as researchers, we need to thoroughly consider the impact on equity of each and every inclusion and exclusion criterion in our studies. Language is an obvious one, but others are subtle. When we don't examine these criteria we risk sustaining racial and ethnic inequities in research participation.
Here’s an interesting case: My dementia study is part of a larger NIH grant at KPWHRI. The principal investigator is KPWHRI senior investigator Robert Penfold, PhD, who is also my mentor in the CATALyST program. While my study focuses on Latinos specifically, the larger study is working with a general population drawn from Kaiser Permanente Washington to study an intervention to help family caregivers attend to relatives with dementia. In my recruiting of participants, I changed a couple of criteria for participating—I removed the language requirement while adding the ethnicity requirement—but otherwise the criteria were the same in the 2 studies. This included a requirement that the participants with dementia had been prescribed an antipsychotic medication for behavioral symptoms of dementia. The prescription serves as a proxy to identify family caregivers who are dealing with challenging behaviors. A goal of the study is to reduce the use of antipsychotics for this indication.
I then encountered a problem that many researchers experience in seeking Latino, Black, or Indigenous participants: After months of trying to recruit Latinos for my study, I had little success. I reviewed the criteria and identified the antipsychotic criterion as a potential problem: It appears that Latino KPWA members are much less likely than non-Latino members to be prescribed an antipsychotic. While future research is needed to test this hypothesis, Rob and I agreed that this criterion was not essential to my study. I have eliminated it for my study in an attempt to identify a larger sample of Latino participants. More careful scrutiny of criteria in advance of recruitment could prevent such unintended consequences.
There are other steps. Oversampling, in which researchers select participants of color so that they comprise a larger share of study enrollment, can have an immediate effect. For the longer term, though, the foundation that underlies all of these efforts is developing a relationship of trust between researchers and communities of color. I know this firsthand. When I first moved to Seattle from Los Angeles, I approached community leaders who have extensive experience working with Latino populations in this area. Even though I myself am a Latina and speak Spanish when I meet them, they still are hesitant to help me to recruit Latino participants for my study. They encourage me to hang out with their community informally and show my face so they can get to know me. Once that relationship is built, and there's trust, then we can talk about research collaborations.
While such changes will take serious effort, they need not take decades and should be adopted now. The benefits to research, to Latino communities and all people of color, and ultimately to our entire society are too important to wait any longer.
healthy findings blog
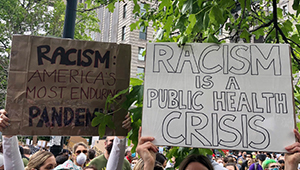
No going back: We must rise now to end structural racism
Dr. Rita Mangione-Smith shares 6 changes our research institute can make to address racism as a public health crisis.
news

Diabetes is more common among minorities at lower weights
At normal weight, Pacific Islanders are 3 times likelier than whites to have diabetes, Kaiser Permanente research finds.
news

Washington state members begin joining the KP research biobank
KPWHRI launches a phone-based recruitment pilot project in May. Outreach to diverse populations is key.
healthy findings blog

How women are breaking academia’s glass ceiling
Dr. Amy Bonomi discusses her new book profiling 23 women who have risen to leadership positions in higher education and how they are changing their institutions.


